Bonyan Organization: Working for a Better Tomorrow
Quick Donation

🚨 Emergency Response for Gaza 🚨
Renewed bombings and blockades intensify Gaza’s humanitarian plight. Essential resources are scarce, homes are destroyed, and basic survival is at risk. The resilience of Gaza’s people is tested amidst these escalating challenges.
A crisis that is not new but is about to take an even more devastating turn.
NEWS

How to Do Zakat Step By Step
Zakat is one of Islam’s 5 pillars and an essential obligation for Muslims with the financial means to perform it. It is a form of charity that is mandatory for sane, adult Muslims who meet certain eligibility criteria. This article will outline the steps to perform zakat in a simple and easy-to-understand manner. Following these […]
The Etiquettes of Giving
The etiquette of giving zakat lies in making the intention (niyyah) before giving it to its recipients. Piety and sincerity are also other preconditions for giving zakat, as it’s an act of worship that requires the purification of the heart in the first place. This article will further explore the etiquette of giving zakat to […]

The Spiritual Significance of Charity During Ramadan
The holy month of Ramadan is highly regarded by Muslims, and it has great value in Islam. It is a month where acts of virtue are encouraged, particularly giving charity to the poor. During this month, we should feel the pain of those in need and increase our virtuous deeds. Thus, Muslims should seize the […]

Ramadan: Empathy, Generosity and Sharing with the Needy
Ramadan is indeed the most ideal time of the year for self-introspection and self-awareness. This process entails an inner process of heart purification which is conducted through fasting not only from food and drink but also from all kinds of worldly, sensual pleasures. In this article, we discuss what role Ramadan plays in cleansing our […]

The Power of Prayer and Charity: How Ramadan Can Transform Our Lives
The holy month of Ramadan provides a great opportunity for Muslims to elevate their spiritual status and go through a process of self-assessment. There are many values that Muslims learn in this blessed month by fasting, such as self-discipline and patience. This article will shed light on the many essential values related to the holy […]
Programs


Early Recovery


Protection and sponsorship
Help our organization by donating today! All donations go directly to making a difference for our


Shelter & non alimentary aid


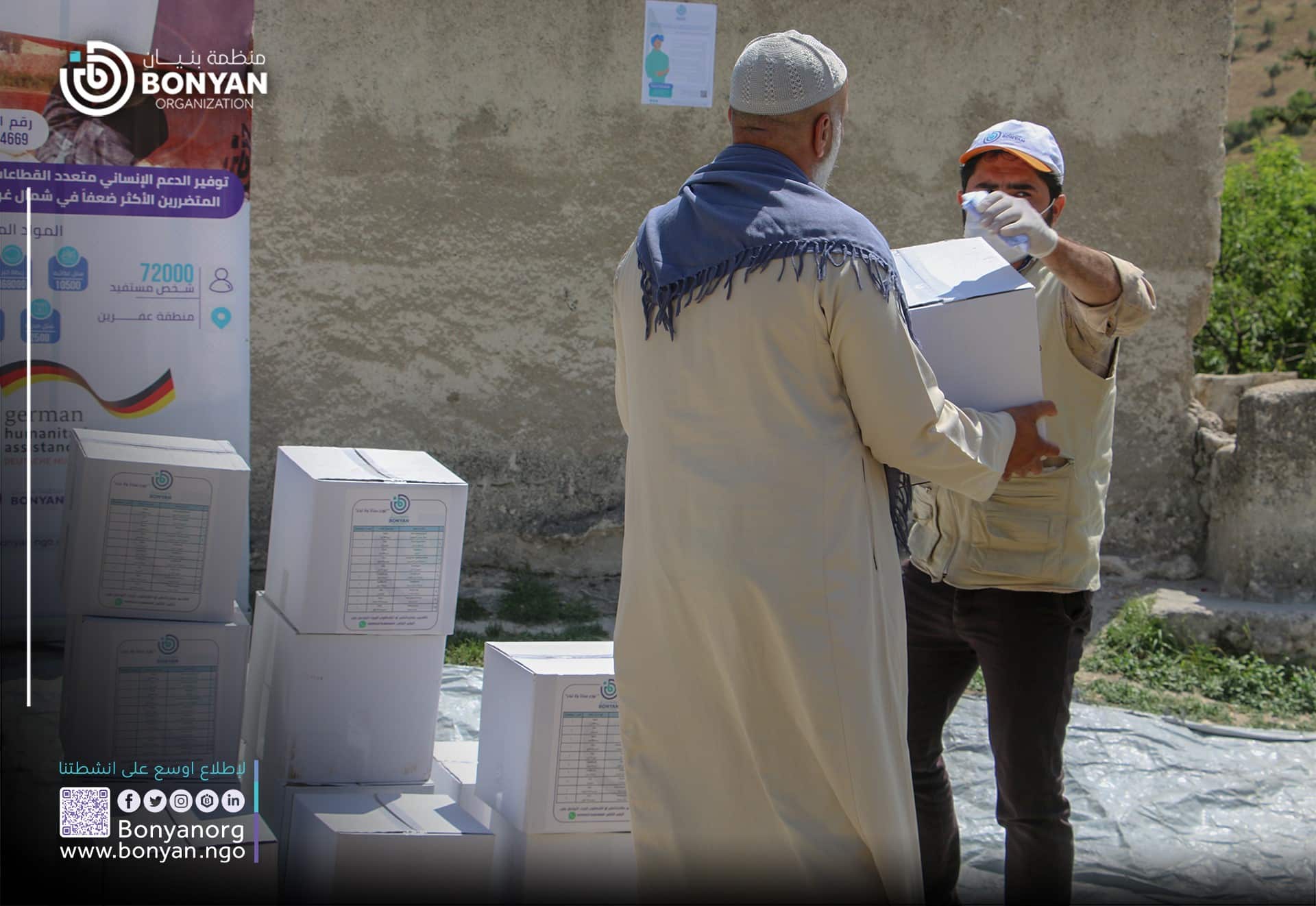
Food Security
Help our organization by donating today! All donations go directly to making a difference for our


Education
Help our organization by donating today! All donations go directly to making a difference for our


Water and sanitation
Help our organization by donating today! All donations go directly to making a difference for our


Emergency Response
Help our organization by donating today! All donations go directly to making a difference for our


Football for Good
Our Partners






Total Beneficaries


















